Spinal Conditions
Scoliosis
Scoliosis is a side to side, three dimensional curve of the spine. Scoliosis is relatively common and occurs in 1 out of 40 people worldwide. Scoliosis impacts every race, every socioeconomic status and every geographical area of the world. In fact, any animal with a spine can develop scoliosis. Scoliosis that progresses to the point of needing treatment is more common in girls than in boys. While there are different causes for scoliosis, most of the time the cause for it is unknown. Newer research is starting to show that scoliosis can run in families but there is not a genetic test just yet to determine exactly who will and will not have scoliosis.
While people are most familiar with three main types of scoliosis, there are actually four types that can develop: congenital, neuromuscular, adolescent idiopathic scoliosis, and adult de novo scoliosis. While these different types have different causes and age groups they affect, they progress similarly.
Although there are still many unanswered questions regarding how and why the bulk of scoliosis cases develop, there are known causes for three of the four main types of the condition: congenital, neuromuscular, and adult denovo scoliosis. The fourth category, idiopathic, is mainly associated with children but can develop in adults as well.
While congenital, neuromuscular and some types of adult-onset denovo scoliosis have known causes, these only make up 20 percent of diagnosed scoliosis cases, and the remaining 80 percent are defined as idiopathic, meaning they have no known single cause.
Congenital, neuromuscular, and idiopathic scoliosis are mainly associated with children.

In addition to this website, you can learn more about scoliosis from the following non-profit.
Congenital Scoliosis
Congenital scoliosis is a spinal deformity that people are born with. In these cases, there is a bone malformation that can cause a scoliosis to develop. Although we understand how incorrect bone formations can cause a spinal deformity, experts are still unsure why people are born with the bone malformation to begin with.
If you think of a healthy spinal cord as rectangles stacked on top of each other like bricks, with congenital scoliosis, one of those bricks is shaped like a triangle and that causes the spine to tilt or curve.

Neuromuscular Scoliosis
Neuromuscular scoliosis develops in children with medical conditions that impair the body’s ability to control the muscles supporting the spine. Some of the most common medical conditions that cause neuromuscular scoliosis to develop include Marfan syndrome, muscular dystrophy, cerebral palsy, and spina bifida.
In most cases of neuromuscular scoliosis, the scoliosis that develops is secondary to the other medical problems the patient has.
Marfan Syndrome
Marfan syndrome is understood as a genetic disorder of the body’s connective tissue. It commonly affects tall and thin people with long limbs. Approximately six out of ten people with Marfan also have scoliosis. While the scoliosis that can develop with Marfan syndrome is not typically severe, a growth spurt in a child with Marfan can cause the scoliosis to progress.

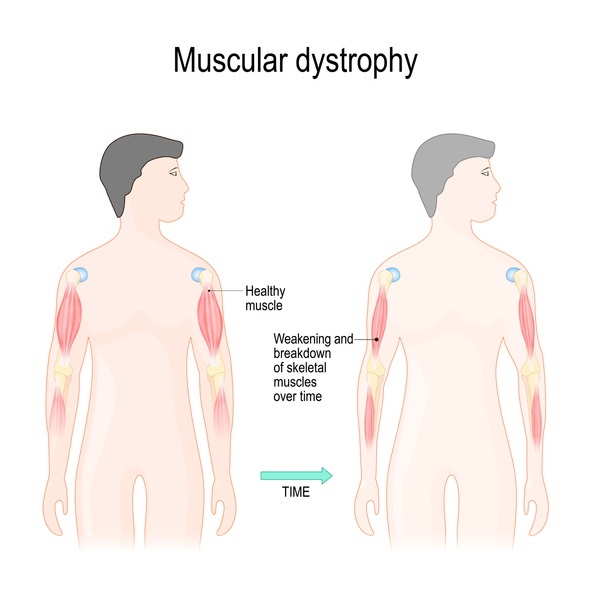
Muscular Dystrophy
Muscular dystrophy (MD) is a rare progressive disease that affects voluntary muscles that control movement of the legs, arms, and trunk. Scoliosis is a common problem for people with muscular dystrophy.
Duchenne MD accounts for 75-to-90 percent of scoliosis cases that develop as a result of the body’s muscle impairment.
Cerebral Palsy
Cerebral Palsy is a condition characterized by impaired muscle coordination. In many cases, cerebral palsy develops in children as a result of brain damage that occurred before or during delivery.
Children with cerebral palsy have significantly elevated chances of developing scoliosis. They are most likely to develop the condition during their early years and into adolescence. The severity of the scoliosis is closely linked to the severity of cerebral palsy and can progress beyond skeletal maturity.

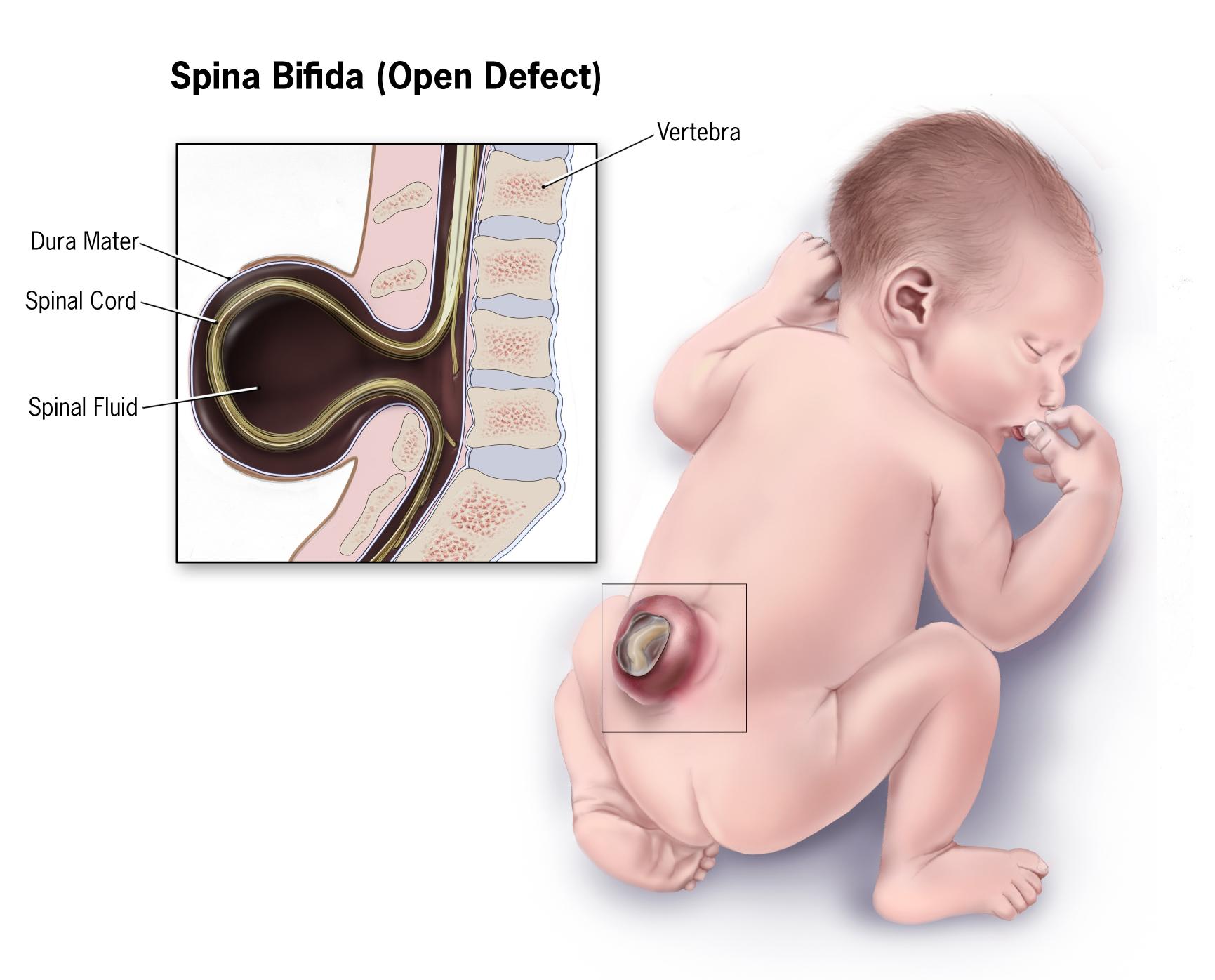
Spina Bifida
Spina bifida is a congenital spinal defect where a gap in the backbone exposes part of the spinal cord and its meninges. It can cause paralysis of the lower limbs and can also affect mental function.
Approximately 50 percent of people with spina bifida will develop scoliosis. Children with spina bifida are at an elevated risk for rapid progression and large spinal curvatures. These patients are monitored closely to watch for progression during growth spurts.
Adolescent Idiopathic Scoliosis
Idiopathic scoliosis can develop in adolescents. The most common age of diagnosis is between 10 and 18. This is the important time when growth spurts take place and the risk of curve progression is high.
AIS is the most common form of the condition, affecting 2-3 percent of adolescents. Idiopathic adolescent scoliosis is more common in females at a ratio of 7:1, and while the reasons aren’t fully understood, a commonly-accepted theory is that it has to do with postural maturity. As females tend to have larger growth spurts in shorter amounts of time, this tendency increases the likelihood of females developing idiopathic adolescent scoliosis.

Adult De Novo Scoliosis (Degenerative Scoliosis)
Adult de novo scoliosis makes up the fourth type of the condition. While many cases of adult scoliosis are extensions of adolescents who weren’t diagnosed and progressed into adulthood with the condition, do novo scoliosis cases are different.
Adults with no history of scoliosis during adolescence who develop the condition fall into the ‘de novo scoliosis’ category. In the majority of these cases, spinal deformities develop because of degenerative changes to the spine that accompany aging.
Degenerative scoliosis occurs in older individuals whose spinal discs are deteriorating due to the natural effects of aging, and this can lead to the development of an abnormal spinal curvature.
Under this umbrella, there are three types of scoliosis that adults can develop: traumatic, pathological, and idiopathic.

Ehlers-Danlos Syndromes
Ehlers-Danlos syndromes (EDS) are a group of connective tissue disorders that affect the body in different ways. EDS is characterized by hyper extensible skin and joint mobility. Scoliosis is a common manifestation of all forms of EDS. Patients who have Kyphoscoliosis EDS may have particularly severe and rapidly- developing curves. Treatment may be focused on preventing progression and alleviating associated signs and symptoms.

Early Onset Scoliosis
Early onset scoliosis (EOS) is defined as spinal curvature before the age of 10. EOS is much rarer and more complex than adolescent idiopathic scoliosis, which is the most common type of scoliosis in kids between the ages of 10 to 18. X-rays are the most common diagnostic measure for EOS. Treatment usually falls into one of four approaches: observation, bracing, casting, surgery. Today’s treatments are highly successful at managing or even correcting EOS.

Traumatic Scoliosis
While experts are unsure of how severe a trauma has to be to cause the development of the condition, accidents can cause spinal deformities to develop.

Adult Idiopathic Scoliosis
While they can develop, instances of adult idiopathic scoliosis are rare. In most cases, as mentioned earlier, they are extensions of AIS cases that went undiagnosed, but of course, these cases are difficult to confirm and track.”

Functional causes of scoliosis
S
How is scoliosis diagnosed?
Scoliosis can be difficult to diagnose. Some spinal curves are visible and obvious, but in other cases, they are not. Curvature of the spine often causes no back pain and usually progresses slowly.
Scoliosis is often overlooked until a child reaches early puberty and starts growing rapidly. But early diagnosis is an important part of successful treatment. For this reason, pediatricians, family physicians, and some school programs routinely look for signs of scoliosis in children and pre-teens.
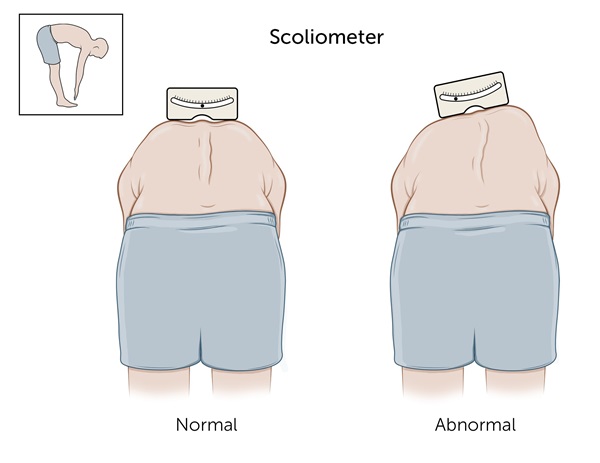
The Adams Forward Bend Test is a common method used to diagnose scoliosis. The patient puts their hands together and bends forward with straight knees, making their spine visible. The clinician looks for unevenness in the hips, ribs, or shoulders. If they see a curve, they may use a scoliometer, a flat piece of metal about the size of an index card, to measure the degree of the curve. A curve of more than five to seven degrees on the scoliometer may indicate scoliosis.
Determining the degree of curvature
If your child has scoliosis, their doctor will gather further information about their spine by asking questions about any family history of scoliosis, doing a physical examination, and looking at an x-ray of the child’s spine. This will help the clinician determine:
- the shape of the curve – whether it is an “S” or “C” shape and whether the ribs and muscles are involved
- the direction of the curve – whether the spine curves to the left, right, or both
- the location of the curve – whether the curve is in the upper or lower spine or both
- the degree of the curve – whether the curve is mild, moderate, or severe”
References:
- https://www.scoliosisreductioncenter.com/blog/what-are-the-4-types-of-scoliosis#:~:text=While%20people%20are%20most%20familiar,they%20progressive%20relatively%20the%20same
- https://www.mayoclinic.org/diseases-conditions/kyphosis/symptoms-causes/syc-20374205#dialogId38018298
- https://www.childrenshospital.org/conditions-and-treatments/conditions/s/scoliosis/diagnosis-and-treatment
